Managing your aging parents’ health? There’s an app for that
September 14, 2023
NYU Meyers’ Tina Sadarangani created a tool to track health and improve communication between caregivers and health providers for older adults
A social worker who works in aging services, Lugo often sees this intergenerational dynamic play out. But she also knows it firsthand, through her experience overseeing the medical needs of her parents who live in Florida, nearly 3,000 miles away from her home in California. With her brother in Massachusetts and her sister in Florida, the siblings have sometimes struggled to keep everyone in the loop on appointments and treatments.
More than three-quarters of adults want to continue living in their homes as they grow older—a practice known as “aging in place.” Family members, friends, home health aides, and health care providers are all often involved in the care for these community-dwelling older adults, but crucial details can easily get lost between them.
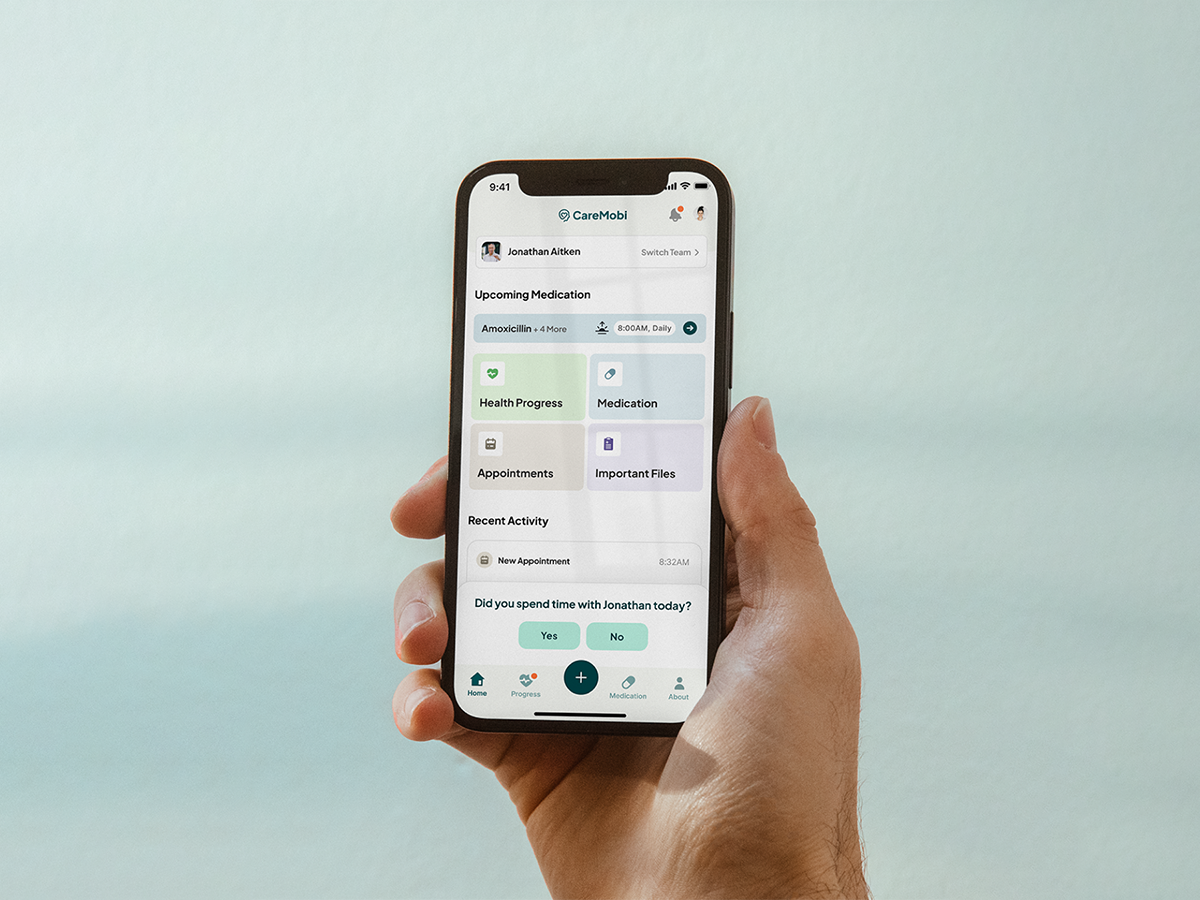
Through her work with older adults and their caregivers, Tina Sadarangani, an assistant professor at NYU Rory Meyers College of Nursing, saw an opportunity to use technology to bridge this gap. Following several years of research and development supported by grants from the National Institute on Aging, Sadarangani created CareMobi, a free smartphone app that connects caregivers with health care providers around the care and wellbeing of older adults.
In CareMobi, users can log important data including a person’s medications, vital signs, appointments, meals and appetite, sleep, and more, and then share this knowledge with their care team within the app.
“Keeping better track of day-to-day health information can help us nip emerging problems in the bud. Our goal is to keep people out of hospitals and emergency rooms by improving communication, and support caregivers as effective advocates by offering data and participating in shared clinical decision making,” says Sadarangani.
Through her mother’s shoulder replacement surgery and her father’s cancer treatment, Lugo has used CareMobi to take notes and provide her family with updates.
“An app like CareMobi is amazing, because if my father has an evaluation next week, I can put that in the app and share it with my siblings. It helps me to communicate what I know to the rest of the family, and they can use it to communicate back,” Lugo says.
One setting that Sadarangani designed CareMobi for is adult day care centers, also known as adult day services or adult day programs, which support the health, nutritional, social, and daily living needs of older adults who live at home. There are roughly 5,000 of these centers in the United States that serve nearly 300,000 frail or disabled adults.
“Professionally, I can see this app really working in our adult day centers,” adds Lugo, who works at Avenidas, which runs a series of programs for community-dwelling older adults in California and has participated in Sadarangani’s research. Lugo noted that adult day care center staff can easily enter a day’s worth of activities to report back to caregivers—including what someone ate that day, what activities they took part in, and any issues that arose.
For her development of CareMobi, Sadarangani was recently selected as a finalist in the National Institute on Aging’s start-up challenge to develop science-driven technologies that address needs related to aging. NYU News spoke with her about managing care for older adults and how families and professionals can help test CareMobi.

Why did you decide to study adult day care centers?
Adult day care centers are essential community resources that enable people to live at home as long as possible and avoid higher levels of care, such as nursing homes. Most importantly, they keep older adults productively engaged—giving them a reason to get up and go somewhere in the morning—which is critical to good health.
Even though people think adult day care centers are for dancing and dominoes, they are staffed by highly knowledgeable, trained professionals—including nurses and social workers—who provide a lot of care, often seeing them four to six hours a day, two to five times a week. The staff really get to know people.
This is important in older adults because often infections and other issues don’t present in typical ways, like they do in other age groups, and you have to look for non-specific signs and symptoms. So when the staff notice that Mr. Smith isn’t acting like himself, they might assess him further and notice that he is asking to the restroom more frequently. They would let the family know that they are concerned he might have a urinary tract infection and request he be seen.
What have you learned about adult day care centers through your initial research?
Our research shows that people who use adult day care centers are often medically complex, have dementia, take more than 12 medications, and may mismanage their medications. These complexities illustrate the important role that these centers and their staff play.
We’ve also done research to figure out how staff at these centers know when there might be a clinical problem, such as an infection, brewing in an older adult. When they start acting funny, the staff become detectives to figure out what’s going on.
No one thinks of adult day centers as being part of the healthcare system, but staff have so much rich information on older adults. It can be hard for them to exchange information with doctors and family caregivers. The staff may try to leave voicemails or send faxes to other providers, or call the person’s caregiver, but it often becomes a game of telephone. By the time they reach a doctor, the older adult has already ended up in the emergency room.
It’s clear that we need a more modern way to help adult day care programs to communicate with caregivers and medical providers. Unlike hospitals, adult day care programs don’t have electronic health records that enable this communication in other settings. Giving staff at adult day centers the tools to be more active members of the care team has the potential to support early clinical intervention and save health care systems lots of money. That’s why we set out to create an app that is responsive to the needs of the teams caring for older adults.
Who did you develop CareMobi for, and how does it work?
CareMobi is a smartphone app that is designed to be a useful, practical tool that connects family caregivers, in-home caretakers, staff at adult day care programs, and medical providers. The goal is to get everyone on the same team, from home health aides to adult children to doctors and nurses.
The app is free and available to anyone who wants to use it. I think it can be really useful for sandwich generation caregivers, like myself, who are juggling the care of both children and their own parents. My father has kidney disease and is on dialysis, and despite the fact that both my parents are doctors and I’m a nurse practitioner, tracking his health is still so hard!
We spent the past few years putting the app together based on our research and talking to a lot of family caregivers and providers. We learned that many caregivers have no idea what to track, so we took the main things that doctors and nurse practitioners ask for at the office, like blood pressure, pain levels, and eating habits, and created ways to log this information in the app and share it with the care team.
Tracking this information enables users to see changes and trends, and hopefully spot something going wrong before it’s too late.
What’s next for the app?
While the beta version of CareMobi is available to anyone, we’re also running a study on its use in adult day care centers. We will very soon be recruiting staff members at adult day care centers, family caregivers, and other care team members to use the app so we can measure if it improves communication and helps to reduce emergency department visits and hospitalizations, particularly in people with dementia.
We expect to learn a lot more about the app and how to better connect care teams in the next six months, and look forward to sharing our findings in 2024.