Jessamin Cipollina, MA
October 27, 2021
Building vaccine confidence is a success challenge for health professionals and community leaders. As trusted professionals, they have the opportunity to influence groups that are more likely to be hesitant to receive vaccines. Building trust about vaccine safety is essential to improving vaccination rates and improving global public health. Nurses, nurse practitioners, midwives, dentists, pharmacists, physicians and physician assistants are among the many health professionals that are well-positioned to foster vaccine confidence in their patients using health literacy to correct misinformation and educate families and communities about the value of vaccines. The COVID-19 and human papillomavirus (HPV) vaccines illustrate the importance of promoting vaccine confidence.
The COVID-19 pandemic has brought to light the impact of vaccine hesitancy and the reasons many people are reluctant to receive any and all vaccines. Vaccine hesitancy refers to those who refuse vaccines despite evidence about safety and availability of vaccines. The We Can Do This campaign launched by the Biden administration aims to dispel myths and misinformation about the COVID-19 vaccine to encourage communities across the US to get vaccinated. Public health campaigns help combat misinformation, thereby improving health literacy and building confidence in individuals to get themselves and their families vaccinated to protect them from potentially fatal infections like COVID-19. Initiatives like the We Can Do This campaign include efforts to spread information and positive messaging about the COVID-19 vaccine through a network of trusted messengers in communities and health care settings, as well as through television ads and across social media platforms.
The momentum behind promoting the COVID-19 vaccine provides an advocacy framework for the HPV vaccine. HPV is responsible for over 34,000 cancer diagnoses every year in the US. Like the COVID vaccine, hesitancy around the HPV vaccine is due to many misconceptions about its safety and social implications. Gardasil 9, the HPV vaccine, has been around for over 15 years; research findings support its safety and effectiveness in preventing HPV and reducing risk for oral cancer. Gardasil 9 prevents 90% of HPV-associated oral, cervical, anal and penile cancers. In 2020, the FDA approved Gardasil 9 as an HPV vaccine for prevention of oropharyngeal and head and neck cancers, making it the only cancer prevention vaccine. The Gardasil 9 vaccine is approved for administration to children as young as age 9 and adults up to age 45. Despite scientific evidence about its effectiveness, only about half of US teens are fully vaccinated. Widespread parental misinformation about its side effects and the erroneous belief that this vaccine promotes sexual behavior among youth contribute to vaccine hesitancy.
Findings from several studies of vaccine hesitancy and parents’ attitudes about the HPV vaccine show that a recommendation from a trusted healthcare provider is the strongest predictor of parents’ decision to have their child receive the vaccine. A recent study from Pediatrics examined HPV vaccine hesitancy among parents using data from the 2021-2018 National Immunization Survey (NIS). Their findings revealed that vaccine hesitancy had increased from 2012-2018 for parents of young girls and boys, and this was largely due to concerns about the safety of the vaccine. A similar study from Lancet, based on NIS data, found that 58% of parents had no intent on having their children vaccinated, citing safety concerns and lack of a provider recommendation as reasons for not having their children vaccinated or completing the HPV vaccine dosage series.
A standard of care for all health care professionals is to provide anticipatory guidance to improve health literacy about vaccines. There is a growing national movement to expand the dental profession’s role in vaccine advocacy and administration. Dental teams have many opportunities to provide information about HPV and the safety of the HPV vaccine to parents of their young patients. Along with HPV vaccine education and recommendation for young patients, dentists perform oral cancer screenings on their adult patients. Early detection of oral HPV infection and cancer has great potential to reduce the spread of HPV as well as the onset of severe HPV-related oral cancers.
Although oral cancer screenings have long been designated to the dental team, medical teams including trusted primary care providers, physicians, physician assistants, pharmacists, nurses, nurse practitioners and community health workers (CHW), need to be knowledgeable about HPV and its oral-systemic links. Management of HPV necessitates interprofessional collaboration across the entire health care team to best address the needs of patients of all ages. Reducing HPV infection and cancer rates requires dental and medical professionals to become well-versed about the importance of the HPV vaccine and provide HPV and oral cancer education resources to their patients and communities. Enhancing the role of all clinicians in providing HPV health literacy beyond the pediatrician’s office is imperative to combating vaccine hesitancy and building vaccine confidence.
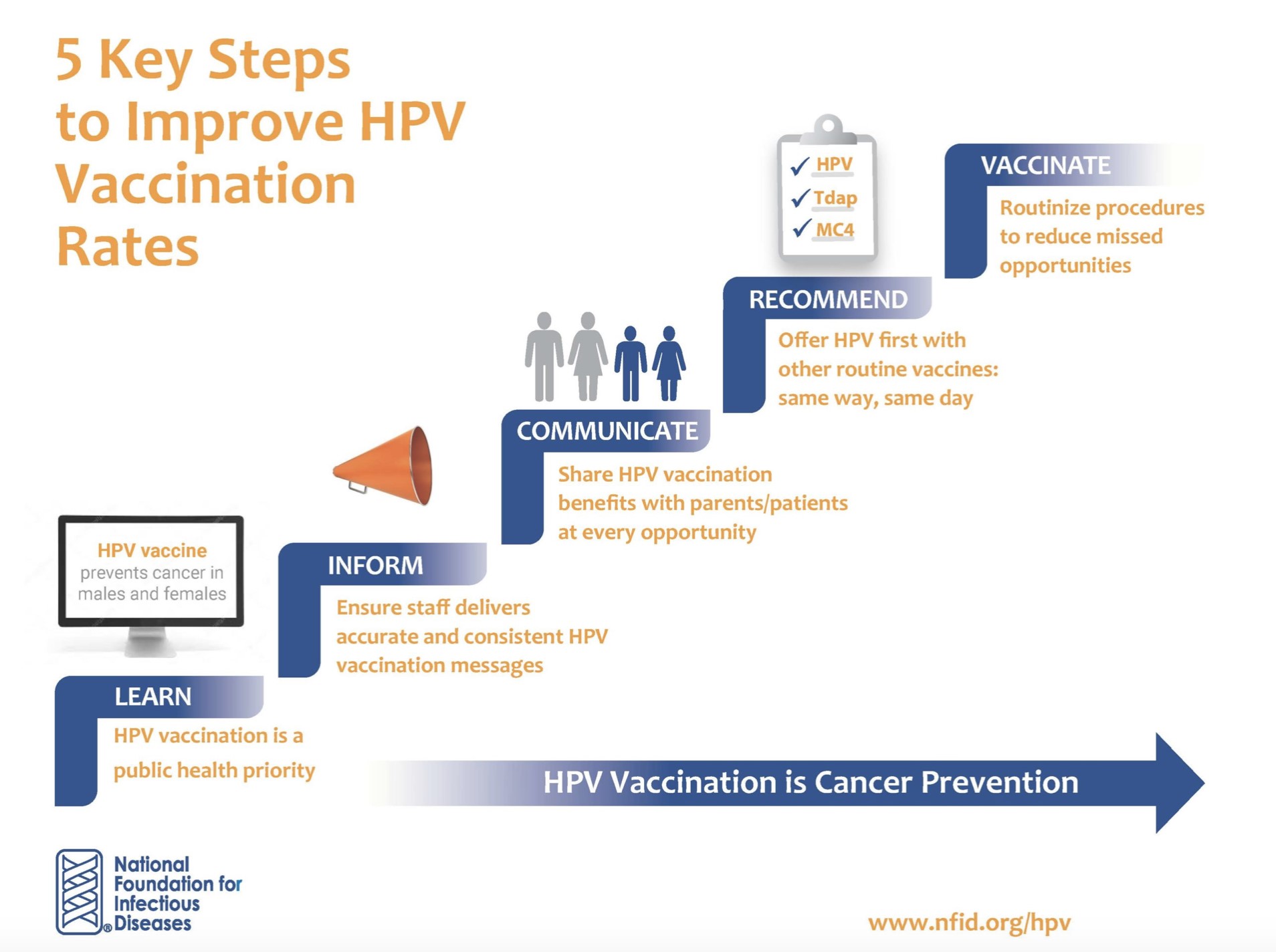
Despite documented progress and success of numerous 20th century life-saving vaccines in eradicating public health crises, vaccine hesitancy has rapidly infiltrated communities worldwide. The explosion of social media and communication technology have provided a platform for spreading misinformation about both the COVID-19 and HPV vaccines, having a negative impact on vaccine confidence. Vaccine hesitancy is a global population health equity problem that demands health professionals provide health literacy and vaccine recommendations to their patients that instill vaccine confidence and trust in health care system. The CDC has numerous resources for clinical teams to use for building HPV vaccine confidence in patients and communities. The following diagram provides a model for steps that clinical teams can take to improve confidence in the HPV and other vaccines.
Sources:
- Badur S, Ota M, Öztürk S, Adegbola R, Dutta A. Vaccine confidence: the keys to restoring trust. Hum Vaccin Immunother, 2020;16(5):1007-1017. doi:10.1080/21645515.2020.1740559
- Centers for Disease Control and Prevention. HPV and Oropharyngeal Cancer. 2020. Updated September 3, 2020.
- Centers for Disease Control and Prevention. Talking to Parents About Infant Vaccines. Updated July 1, 2019.
- Centers for Disease Control and Prevention. Top 10 Tips for HPV Vaccination Success: Attain and Maintain High HPV Vaccination Rates. Updated April 7, 2017.
- Haber J, Hartnett E, Feldman LM, Cipollina JE. Making the case for interprofessional education and practice collaboration to address rising rates of HPV-associated oropharyngeal cancers. J Dent Educ, 2022;86(1):47-50. doi: 10.1002/jdd.12752.
- Johnson D. VP Kamala Harris, HHS open drive to inspire Americans to take COVID-19 vaccine. Published April 1, 2021.
- Mehra S. FDA expands Gardasil 9 approval for head and neck cancer prevention. Published June 15, 2020.
- Sonawane K, Zhu Y, Lin Y et al. HPV vaccine recommendations and parental intent. Pediatrics, 2021:147(3). doi: 10.1542/peds.2020-026286.
- Sonawane K, Zhu Y, Montealegre JR et al. Parental intent to initiate and complete the human papillomavirus vaccine series in the USA: a nationwide, cross-sectional survey. Lancet, 2020;5(9):484-492. doi: 10.1016/S2468-2667(20)30139-0