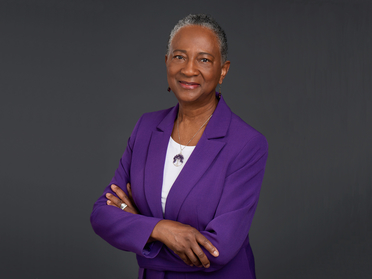
Jamesetta A Newland
PhD DPNAP FNP-BC FAAN FAANP
Clinical Professor Emerita
jan7@nyu.edu
1 212 998 5319
433 FIRST AVENUE
NEW YORK, NY 10010
United States
Jamesetta A Newland's additional information
-
-
Prof. Jamesetta (Jamie) Newland is Clinical Professor Emerita at NYU Rory Meyers College of Nursing. A strong proponent of faculty practice, she spent much of her clinical practice in nurse-managed health centers (NMHCs), holding positions as direct care nurse practitioner (NP), administrative director, and consultant to other academic nursing schools on NMHCs and faculty practice. She has taught master's and doctoral students since 1993. Considered an expert in NP education and practice, her services have been sought internationally by schools of nursing in Botswana, China, Japan, and Lithuania, and she was instrumental in establishing the first advanced nursing practice master's programs in Japan and Lithuania. She is a Certified Global Nurse Consultant with the International Council of Nurses (ICN) and the Commission on Graduates of Foreign Nursing Schools (CFGSN).
Newland has numerous scholarly publications to her credit and has been the editor-in- chief of The Nurse Practitioner journal for many years. She spends most of her time participating in professional organizations and remains committed to lifelong learning. She promotes building partnerships with patients to provide the best care. Social justice is central to her work, which she instills in the next generation of nurses through ongoing mentorship, developing future leaders who are driven to address inequity and disparities in health and all areas of the human experience.
-
-
PhD, University of PennsylvaniaPost-Master’s Certificate in Teaching, University of PennsylvaniaMS, Pace UniversityBA, Gustavus Adolphus College
-
-
Faculty practiceFamiliesGlobalHealth EquityNursing educationPrimary careWomen's health
-
-
American Academy of Nursing: FellowAmerican Association of Nurse Practitioners: FellowAmerican Nurses AssociationANA NYAssociation for the Advancement of Baltic StudiesBlack Alumni Society of NYC – University of PennsylvaniaCommittee on Publication Ethics - COPEEastern Nursing Research SocietyFulbright Alumni Association (Fulbright Specialist Roster, 2016-2023)International Association of Sickle Cell Nurses and Professional AssociatesInternational Society of Nurses in GeneticsLienhard School of Nursing Alumni AssociationNational Academies of Practice: Distinguished Practitioner and FellowNational Black Nurses Association: Fellow, Academy of Diversity Leaders in NursingNational Conference for Nurse Practitioners, Planning Panel, Wolters Kluwer HealthNational League for NursingNational Nursing Leadership Board, Gustavus Adolphus CollegeNational Organization of Nurse Practitioner FacultiesNew York Academy of Medicine: FellowNew York State, Board of Nursing, Member (2017-2022) (2022-2027)Nurse Practitioners of New YorkPenn Nursing Alumni AssociationSigma Theta Tau International – Zeta-Omega-at-Large and Xi Chapters
-
-
Faculty Honors Awards
Lifetime Achievement Award, National Organization of Nurse Practitioner Faculties (2025)Distinguished Alumni Citation, Gustavus Adolphus College (2024)Luminary Fellow [inaugural], Academy of Diversity Leaders in Nursing, National Black Nurses Association (2024)Fellow, American Academy of Nursing (2017)Legacy Award, Estelle Osborne, NYU Meyers (2017)Fellow, New York Academy of Medicine (2017)Fulbright Specialist Roster (2016)25 Top Nurse Practitioner Program Professors, NursePractitionerSchools.com (2014)Outstanding Alumni Award, Department of Nursing, Gustavus Adolphus College (2012)Nurse Practitioner Award for Excellence, New York State, American Academy of Nurse Practitioners (2011)Excellence in Social Justice Award, Pace University (2007)Distinguished Practitioner and Fellow, Nursing, National Academies of Practice (2005)Fellow, American Academy (Association) of Nurse Practitioners (2005)Emily Bissell Award, American Lung Association (2004)National Role Model, Minority Access, Inc. (2002)Nurse Scholar of the Year, Sigma Theta Tau, Zeta Omega-At-Large (2001) -
-
Publications
Janus : Remembering the past and looking to the future
AbstractNewland, J. (2024). In Nurse Practitioner (Vols. 49, Issue 1, p. 4). 10.1097/01.NPR.0000000000000133Abstract~Older people’s experience and related factors while receiving home-based long-term care services : a qualitative study
AbstractNorvilaitė, A., Newland, J., & Blaževičienė, A. (2024). In BMC Nursing (Vols. 23, Issue 1). 10.1186/s12912-024-02234-yAbstractBackground: Home-based care may cover anything from 24-hour support for people with a disability, to short-term post-discharge care, or to periodic assistance with simple tasks such as domestic aid for frail older people. The process can be complex and time-consuming and requires coordination between the individual, their family caregivers, and healthcare providers. Receiving care at home can also lead to social isolation as older people may have limited opportunities for social interaction. This study aimed to investigate older people’s experience and related factors while receiving home-based long-term care services. Methods: A qualitative study was used. Face-to-face individual interviews were conducted with people who were receiving nursing care in their homes (N = 17) and analyzed through thematic analysis. Results: Analysis of interview data resulted in the identification of three major themes that captured participants’ personal experiences regarding long-term care in the home: (1) Challenges faced by older people receiving long-term care at home; (2) The impact of home care services on people’s social well-being; and (3) Older people’s contradictory emotions regarding care delivery. Conclusions: Findings of the study revealed that the most important and challenging factors in home care from the perspective of older people were social well-being, religious needs, and physical needs. They considered the nurses who provided these services as family members and the most significant helpers in their daily activities. Participants expressed a desire for more services in the future.Public health in the US : Not quite universal coverage
AbstractNewland, J. (2024). In The Nurse practitioner (Vols. 49, Issues 8, p. 7). 10.1097/01.NPR.0000000000000214Abstract~What makes nursing art?
AbstractNewland, J. (2024). In Nurse Practitioner (Vols. 49, Issues 4, p. 6). 10.1097/01.NPR.0000000000000169Abstract~Black history and nursing : Finding an unexpected connection
AbstractNewland, J. (2023). In Nurse Practitioner (Vols. 48, Issues 2, p. 5). 10.1097/01.NPR.0000000000000009Abstract~Finding a way to be a nurse day after day
AbstractNewland, J. (2023). In Nurse Practitioner (Vols. 48, Issues 5, p. 6). 10.1097/01.NPR.0000000000000042Abstract~#HealthForAll in today's world
AbstractNewland, J. (2023). In Nurse Practitioner (Vols. 48, Issues 4, p. 5). 10.1097/01.NPR.0000000000000030Abstract~A lasting impact : Remembering an NP icon
AbstractNewland, J. (2023). In Nurse Practitioner (Vols. 48, Issues 9, pp. 6-7). 10.1097/01.NPR.0000000000000092Abstract~Making healthcare possible for Earth's 8 billion people
AbstractNewland, J. (2023). In Nurse Practitioner (Vols. 48, Issues 8, p. 6). 10.1097/01.NPR.0000000000000081Abstract~The need for NPs will never end
AbstractNewland, J. (2023). In Nurse Practitioner (Vols. 48, Issues 11, p. 6). 10.1097/01.NPR.0000000000000108Abstract~ -
-
Active Projects