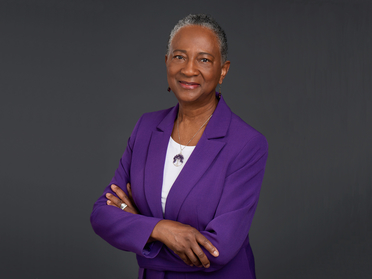
Jamesetta A Newland
PhD DPNAP FNP-BC FAAN FAANP
Clinical Professor Emerita
jan7@nyu.edu
1 212 998 5319
433 FIRST AVENUE
NEW YORK, NY 10010
United States
Jamesetta A Newland's additional information
-
-
Prof. Jamesetta (Jamie) Newland is Clinical Professor Emerita at NYU Rory Meyers College of Nursing. A strong proponent of faculty practice, she spent much of her clinical practice in nurse-managed health centers (NMHCs), holding positions as direct care nurse practitioner (NP), administrative director, and consultant to other academic nursing schools on NMHCs and faculty practice. She has taught master's and doctoral students since 1993. Considered an expert in NP education and practice, her services have been sought internationally by schools of nursing in Botswana, China, Japan, and Lithuania, and she was instrumental in establishing the first advanced nursing practice master's programs in Japan and Lithuania. She is a Certified Global Nurse Consultant with the International Council of Nurses (ICN) and the Commission on Graduates of Foreign Nursing Schools (CFGSN).
Newland has numerous scholarly publications to her credit and has been the editor-in- chief of The Nurse Practitioner journal for many years. She spends most of her time participating in professional organizations and remains committed to lifelong learning. She promotes building partnerships with patients to provide the best care. Social justice is central to her work, which she instills in the next generation of nurses through ongoing mentorship, developing future leaders who are driven to address inequity and disparities in health and all areas of the human experience.
-
-
PhD, University of PennsylvaniaPost-Master’s Certificate in Teaching, University of PennsylvaniaMS, Pace UniversityBA, Gustavus Adolphus College
-
-
Faculty practiceFamiliesGlobalHealth EquityNursing educationPrimary careWomen's health
-
-
American Academy of Nursing: FellowAmerican Association of Nurse Practitioners: FellowAmerican Nurses AssociationANA NYAssociation for the Advancement of Baltic StudiesBlack Alumni Society of NYC – University of PennsylvaniaCommittee on Publication Ethics - COPEEastern Nursing Research SocietyFulbright Alumni Association (Fulbright Specialist Roster, 2016-2023)International Association of Sickle Cell Nurses and Professional AssociatesInternational Society of Nurses in GeneticsLienhard School of Nursing Alumni AssociationNational Academies of Practice: Distinguished Practitioner and FellowNational Black Nurses Association: Fellow, Academy of Diversity Leaders in NursingNational Conference for Nurse Practitioners, Planning Panel, Wolters Kluwer HealthNational League for NursingNational Nursing Leadership Board, Gustavus Adolphus CollegeNational Organization of Nurse Practitioner FacultiesNew York Academy of Medicine: FellowNew York State, Board of Nursing, Member (2017-2022) (2022-2027)Nurse Practitioners of New YorkPenn Nursing Alumni AssociationSigma Theta Tau International – Zeta-Omega-at-Large and Xi Chapters
-
-
Faculty Honors Awards
Lifetime Achievement Award, National Organization of Nurse Practitioner Faculties (2025)Distinguished Alumni Citation, Gustavus Adolphus College (2024)Luminary Fellow [inaugural], Academy of Diversity Leaders in Nursing, National Black Nurses Association (2024)Fellow, American Academy of Nursing (2017)Legacy Award, Estelle Osborne, NYU Meyers (2017)Fellow, New York Academy of Medicine (2017)Fulbright Specialist Roster (2016)25 Top Nurse Practitioner Program Professors, NursePractitionerSchools.com (2014)Outstanding Alumni Award, Department of Nursing, Gustavus Adolphus College (2012)Nurse Practitioner Award for Excellence, New York State, American Academy of Nurse Practitioners (2011)Excellence in Social Justice Award, Pace University (2007)Distinguished Practitioner and Fellow, Nursing, National Academies of Practice (2005)Fellow, American Academy (Association) of Nurse Practitioners (2005)Emily Bissell Award, American Lung Association (2004)National Role Model, Minority Access, Inc. (2002)Nurse Scholar of the Year, Sigma Theta Tau, Zeta Omega-At-Large (2001) -
-
Publications
The epidemic of gun violence in America
AbstractNewland, J. (2021). In Nurse Practitioner (Vols. 46, Issues 6, p. 10). 10.1097/01.NPR.0000751800.62349.8eAbstract~Integration of Physical and Psychiatric Assessment
AbstractDoran, V. C., & Newland, J. (2021). In Child and Adolescent Behavioral Health : A Resource for Advanced Practice Psychiatric and Primary Care Practitioners in Nursing (pp. 58-89). Wiley. 10.1002/9781119487593.ch4AbstractThis chapter describes the elements that make up a comprehensive psychiatric-mental health assessment of children and adolescents. This assessment can be used in primary care settings to help identify children and adolescents in need of mental health services. Key areas include history taking, physical examination process, risk, protective factors, teaching needs of the child or adolescent and family, and ways to communicate the assessment findings to the patient and family and, if appropriate, the school so that they are able to pursue appropriate treatment as needed. The chapter provides advanced practice registered nurses and other primary care practitioners (PCPs) in primary care and mental health settings with a way to systematically approach the assessment of the behavioral and mental health of their patients. It aims to assist PCPs with the knowledge and confidence to proceed with their evaluation of the child's history, behavior, complaints, school performance, social skills, family functioning, and available resources for care.Integration of physical and psychiatric assessment
AbstractDoran, V. C., & Newland, J. (2021). In E. L. Yearwood, G. S. Pearson, & J. A. Newland (Eds.), Child and adolescent behavioral health : A resource for advanced practice psychiatric and primary care practitioners in nursing (second, pp. 58-89). John Wiley and Sons.Abstract~The nurturing intent of nature
AbstractNewland, J. (2021). In Nurse Practitioner (Vols. 46, Issues 10, p. 9). 10.1097/01.NPR.0000790512.02956.efAbstract~Preface to Second Edition
AbstractYearwood, E. L., Pearson, G. S., & Newland, J. (2021). In Child and Adolescent Behavioral Health : A Resource for Advanced Practice Psychiatric and Primary Care Practitioners in Nursing (p. xvii-xviii). Wiley.Abstract~Preventing foodborne illnesses
AbstractNewland, J. (2021). In Nurse Practitioner (Vols. 46, Issues 9, p. 9). 10.1097/01.NPR.0000769772.98227.0bAbstract~Seeking a different 2021
AbstractNewland, J. (2021). In Nurse Practitioner (Vols. 46, Issue 1, p. 5). 10.1097/01.NPR.0000724524.61632.a0Abstract~We stand on the shoulders of women past
AbstractNewland, J. (2021). In Nurse Practitioner (Vols. 46, Issues 3, p. 5). 10.1097/01.NPR.0000733680.25240.9cAbstract~Why are nurses still asking when?
AbstractLaskowski-Jones, L., & Newland, J. (2021). In Nursing (Vols. 51, Issues 12, pp. 6-7). 10.1097/01.NURSE.0000800140.35986.f0Abstract~Why are nurses still asking when?
AbstractNewland, J. (2021). In Nurse Practitioner (Vols. 46, Issues 7, p. 9). 10.1097/01.NPR.0000753868.12534.8aAbstract~ -
-
Active Projects